PROTECT YOUR DNA WITH QUANTUM TECHNOLOGY
Orgo-Life the new way to the future Advertising by AdpathwayA groundbreaking study published recently has illuminated a promising new therapeutic avenue for osteoarthritis, a debilitating joint disease that affects millions worldwide. Researchers have uncovered that fexofenadine, a widely used antihistamine, may hold substantial potential in halting and even reversing the progression of osteoarthritis by manipulating key molecular pathways fundamental to cartilage metabolism. This discovery could transform the management of osteoarthritis, shifting from symptomatic relief towards true disease modification.
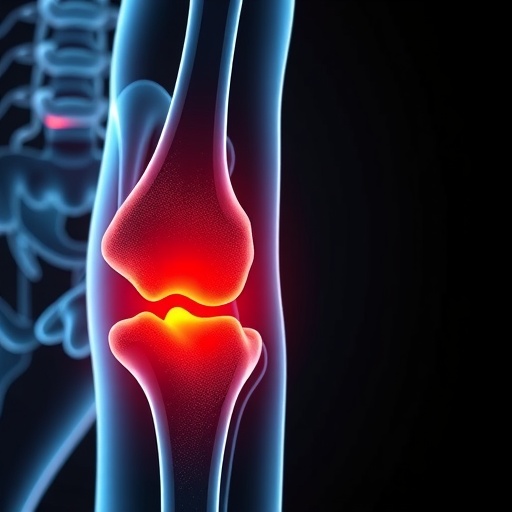
Osteoarthritis, characterized by the gradual degeneration of cartilage and joint inflammation, leads to debilitating pain and loss of mobility. The intricate balance between anabolic and catabolic processes within the cartilage matrix governs joint health; disturbances in these processes result in cartilage breakdown and disease advancement. Historically, treatments have targeted symptom relief without significantly altering the underlying molecular mechanisms. However, the study led by Liu et al. brings forth a novel strategy by utilizing fexofenadine’s unexpected molecular targets to restore this fragile equilibrium.
Fexofenadine, traditionally prescribed to alleviate allergic symptoms by blocking histamine receptors, was scrutinized for its off-target effects on cartilage. Through rigorous biochemical and cellular analysis, the researchers revealed that fexofenadine modulates the activity of two critical signaling molecules: Smad2 and STAT1. These transcription factors are pivotal in regulating genes responsible for anabolic activities within chondrocytes, the cells that maintain cartilage integrity. By enhancing Smad2 and inhibiting STAT1, fexofenadine promotes cartilage regeneration and suppresses inflammatory catabolic pathways.
The study further demonstrated that fexofenadine binds to cytosolic phospholipase A2 (cPLA2), an enzyme intricately involved in the synthesis of pro-inflammatory lipid mediators. The inhibition of cPLA2 activity by fexofenadine significantly reduced the catabolic and inflammatory responses in cartilage tissue samples. This dual mechanism of action—stimulating anabolic gene expression via Smad2 activation and curbing catabolic damage through cPLA2 inhibition—underpins the robust chondroprotective effects observed in experimental models.
Using in vivo osteoarthritis models, the authors validated their molecular findings, showing that systemic administration of fexofenadine not only alleviated joint inflammation but also preserved cartilage architecture. Histological analyses revealed significant reduction in cartilage erosion and preservation of extracellular matrix components essential for joint function. These outcomes suggest a disease-modifying capacity that extends beyond the drug’s conventional use.
The implications of targeting Smad2 and STAT1 extend far beyond osteoarthritis, as these factors play central roles in various fibrotic and inflammatory conditions. By repositioning fexofenadine, a drug with well-characterized safety profiles, the research circumvents the protracted timelines typically associated with novel drug development. This drug repurposing strategy accelerates the pathway towards clinical application, bringing hope to patients suffering from chronic degenerative joint diseases.
Crucially, the research also elucidates the interplay between anabolic and catabolic pathways in cartilage homeostasis, providing fresh insights into the molecular underpinnings that drive osteoarthritis progression. This knowledge may spur the development of combination therapies that synergistically modulate these pathways for enhanced therapeutic efficacy.
Despite these promising findings, the researchers emphasize the need for rigorous clinical trials to determine optimal dosing regimens, long-term efficacy, and safety of fexofenadine as an osteoarthritis treatment. Potential off-target effects, especially given the drug’s broad biological activity, require thorough evaluation to ensure patient safety in chronic usage.
Future investigations may also explore how genetic variations in Smad2, STAT1, and cPLA2 pathways influence patient responsiveness to fexofenadine treatment, paving the way for personalized medicine approaches in osteoarthritis management. Such precision therapeutics could maximize benefit while minimizing adverse effects.
Moreover, the study reopens intriguing questions about the roles of histamine receptor antagonists in musculoskeletal health beyond their established applications. Could other antihistamines exhibit similar chondroprotective effects, or is fexofenadine uniquely suited due to its interaction with intracellular signaling networks? These avenues merit exploration.
As we await clinical validation, this research underscores a pivotal shift in osteoarthritis therapy—moving from symptomatic suppression to molecular targeting that restores joint tissue equilibrium. A common allergy medication might soon become a frontline treatment against a major cause of disability worldwide.
Given the global burden of osteoarthritis, the translational potential of this discovery is profound. If successful in clinical practice, fexofenadine could significantly reduce the need for invasive surgeries, such as joint replacements, thus decreasing healthcare costs and improving quality of life for millions.
In summary, Liu and colleagues’ study adds a vital piece to the osteoarthritis puzzle by demonstrating that fexofenadine’s interaction with Smad2, STAT1, and cPLA2 orchestrates a favorable anabolic-catabolic balance in cartilage. This novel mechanism heralds new hope for developing effective, safe, and readily available treatments for a disease long deemed incurable.
As the scientific and medical communities deepen their understanding of these complex molecular pathways, innovative therapies like this one pave the way for a future where osteoarthritis progression can be effectively managed, or even halted. The convergence of drug repurposing and molecular biology in this research exemplifies the power of interdisciplinary innovation in tackling chronic diseases.
This study not only shines a spotlight on a familiar drug’s unexpected capabilities but also inspires confidence that nature’s existing pharmacopeia may hold answers to some of medicine’s most intractable problems—answers waiting to be uncovered through cutting-edge research.
Subject of Research: Osteoarthritis therapy through molecular targeting of chondrocyte anabolic and catabolic pathways using fexofenadine.
Article Title: Fexofenadine protects against osteoarthritis by targeting Smad2 and STAT1 to enhance anabolism and binding cPLA2 to inhibit catabolism.
Article References:
Liu, K., Zhang, X., Ning, B. et al. Fexofenadine protects against osteoarthritis by targeting Smad2 and STAT1 to enhance anabolism and binding cPLA2 to inhibit catabolism. Cell Death Discov. 11, 473 (2025). https://doi.org/10.1038/s41420-025-02754-9
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41420-025-02754-9
Tags: antihistamine repurposing for arthritiscartilage degeneration and inflammationdisease modification for osteoarthritisfexofenadine for osteoarthritis treatmentfexofenadine’s off-target effectsimproving mobility in osteoarthritis patientsmolecular pathways in osteoarthritis managementnovel therapeutic approaches for joint diseasesresearch on joint disease therapiesrestoring cartilage balance with drugsSTAT1 modulation in cartilage metabolismtargeting Smad2 in joint health


 11 hours ago
8
11 hours ago
8



















 English (US) ·
English (US) ·  French (CA) ·
French (CA) ·