PROTECT YOUR DNA WITH QUANTUM TECHNOLOGY
Orgo-Life the new way to the future Advertising by AdpathwayA groundbreaking study published in the journal Engineering has leveraged advanced machine learning methodologies to unravel the complex heterogeneity of chronic obstructive pulmonary disease (COPD) among Chinese patients. By harnessing a national-scale dataset derived from the Enjoying Breathing Program, this research not only categorizes COPD patients into clinically significant clusters but also deciphers how varying comorbidity profiles uniquely affect health-related quality of life (HRQoL). This work illuminates the path toward precision public health strategies tailored to the intricate interplay between COPD and its common comorbidities.
COPD, a chronic and progressive respiratory condition, maintains its position as a leading cause of morbidity and mortality globally, ranking fourth in worldwide death causes as of 2021. Characterized predominantly by persistent and irreversible airflow obstruction, this disease also exhibits marked heterogeneity in clinical presentation and progression. The burden of COPD in China alone is substantial, with epidemiological surveys like the China Pulmonary Health Study indicating a prevalence of approximately 8.6% among adults aged 20 years and above. The complexity of COPD is further compounded by frequent co-occurrence with systemic comorbidities such as cardiovascular diseases, asthma, bronchiectasis, and metabolic disorders including diabetes, each of which profoundly shapes the patient’s prognosis and overall quality of life.
To dissect this multifaceted clinical landscape, the research team employed a comprehensive cross-sectional design, incorporating data from over 11,000 COPD patients enrolled between 2020 and 2023 in the Enjoying Breathing Program. Notably, about 59% of these participants presented with at least one comorbid condition, reflecting the real-world burden of multimorbidity in COPD populations. Health-related quality of life was meticulously assessed using the EQ-5D-5L instrument, a validated tool that quantifies patient-perceived health status across dimensions such as mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.
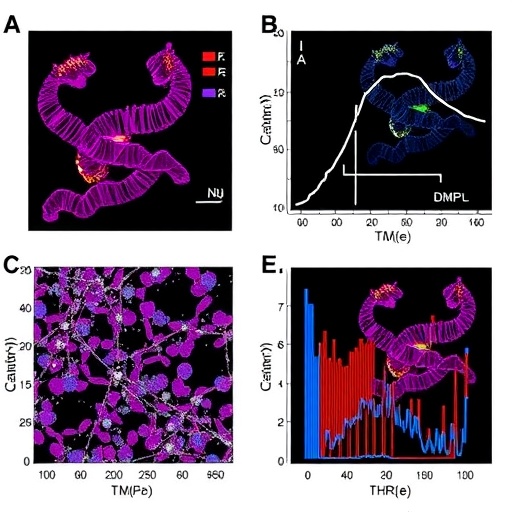
A key methodological innovation in this study was the application of multiple correspondence analysis (MCA) to distill 31 input variables—including 27 distinct comorbidities alongside socio-demographic and health-related characteristics—into three principal, uncorrelated components. This dimensionality reduction step was critical in managing the complexity of the dataset and preparing it for sophisticated cluster analysis. Subsequently, the researchers deployed unsupervised machine learning algorithms, specifically the enhanced K-means++ clustering method paired with hierarchical clustering approaches, to uncover latent patient subgroups within this high-dimensional data space.
The analytic framework yielded four robust and clinically interpretable COPD patient clusters. The largest cluster, labeled “young male smokers,” predominantly comprised younger male patients with a high prevalence of current and former smoking but relatively low comorbidity burden. This group’s profile aligns with classical etiological drivers of COPD and suggests a more straightforward disease phenotype. In stark contrast, the “biomass-exposed females” cluster, characterized by a majority of women with minimal smoking history but significant exposure to biomass fuel smoke, highlights alternative environmental risk factors, underscoring COPD’s diverse etiologic spectrum.
Two additional clusters reflected more severe and complex disease states. The “respiratory comorbidity” group exhibited the worst lung function metrics and a predominance of chronic bronchitis and pulmonary emphysema, underscoring advanced disease pathology compounded by respiratory complications. Meanwhile, the “elderly multimorbid” cluster consisted mostly of patients aged 70 years or older, with high prevalence rates of systemic comorbidities such as hypertension, ischemic heart disease, and diabetes, painting a picture of compounded vulnerability due to aging and multimorbidity.
Crucially, the study established a clear gradient of health-related quality of life deterioration across these clusters. While the young male smokers reported the highest EQ-5D-5L utility scores, averaging 0.74, clusters marked by respiratory complications and multimorbidity had significantly lower scores, 0.66 and 0.65 respectively, indicating impaired quality of life. The respiratory comorbidity cluster not only demonstrated the poorest overall outcomes but also bore elevated risks of mobility limitations, difficulties in performing daily activities, and psychological distress manifested as anxiety and depression. The elderly multimorbid group similarly suffered from pronounced deficits in mobility and experienced greater pain and discomfort.
These findings illuminate the necessity for nuanced, cluster-tailored intervention strategies in COPD management. The marked differences in comorbidity composition and corresponding HRQoL across clusters advocate for integrated care models that transcend conventional monolithic treatment paradigms. Specifically, the data suggest that public health policies and clinical pathways need to be sensitively calibrated to address specific risk exposures—such as tobacco smoking or biomass fuel use—and manage coexisting chronic conditions that magnify disease burden.
This pioneering application of machine learning in a large-scale, multicenter COPD cohort establishes a new paradigm for epidemiological research and precision medicine in respiratory health. By discerning actionable patient subgroups grounded in multimorbidity profiles and quality-of-life outcomes, this work equips clinicians and policymakers with refined tools to optimize resource allocation, personalize treatment regimens, and ultimately enhance patient-centered outcomes.
Further research directions proposed by the authors include the validation of these clusters in independent cohorts and longitudinal settings, to confirm stability and predictive utility over time. Incorporating genetic, biomarker, and environmental exposure data could further enrich cluster definitions and mechanistic insights. The potential scalability of this analytical framework to other chronic diseases characterized by phenotypic heterogeneity also portends broad applicability in medical research.
The ethical rigor underpinning this investigation, compliant with the Declaration of Helsinki and approved by the China–Japan Friendship Hospital, reinforces its scientific credibility. In addition, the study’s registration at ClinicalTrials.gov adds transparency and adherence to best research practices.
In summarizing, this study heralds a transformative leap forward in understanding COPD’s multifactorial nature within China’s diverse populations. The integration of advanced computational methods, robust clinical data, and comprehensive health quality metrics provides a compelling template for future endeavors aiming to unravel the complexity of chronic diseases. As COPD continues to impose significant demands on global health systems, such insightful stratification of patient populations is pivotal to ushering in an era of personalized, efficacious care.
Subject of Research: Chronic Obstructive Pulmonary Disease (COPD) patient clustering and health-related quality of life impact analysis using machine learning.
Article Title: Exploring COPD Patient Clusters and Associations with Health-Related Quality of Life Using A Machine Learning Approach: A Nationwide Cross-Sectional Study
Web References:
Full article: https://doi.org/10.1016/j.eng.2025.05.005
Journal website: https://www.sciencedirect.com/journal/engineering
Image Credits: Chao Wang, Fengyun Yu, Zhong Cao, Ke Huang, Qiushi Chen, Pascal Geldsetzer, Jinghan Zhao, Zhoude Zheng, Till Bärnighausen, Ting Yang, Simiao Chen, Chen Wang
Keywords: Health and medicine, Chronic obstructive pulmonary disease, Machine learning, Patient clusters, Comorbidity, Quality of life, COPD heterogeneity, Public health interventions
Tags: chronic obstructive pulmonary disease studychronic respiratory condition managementcomorbidities and COPDCOPD and cardiovascular diseasesCOPD morbidity and mortalityCOPD patient prognosis and quality of lifeCOPD patient subgroups Chinahealth-related quality of life COPDmachine learning in healthcarenational dataset COPD researchprecision public health strategiesrespiratory disease epidemiology


 8 hours ago
12
8 hours ago
12



















 English (US) ·
English (US) ·  French (CA) ·
French (CA) ·