PROTECT YOUR DNA WITH QUANTUM TECHNOLOGY
Orgo-Life the new way to the future Advertising by AdpathwayIn the dynamic realm of oncology, the advent of targeted radionuclide therapy (TRT) marks a paradigm shift that fuses precision molecular targeting with the destructive power of radiotherapy. This innovative therapeutic approach has rapidly evolved from conceptual frameworks to clinical realities, offering a transformative modality that selectively delivers cytotoxic radiation to malignancies, thereby sparing healthy tissue and minimizing systemic toxicity. Over the past several decades, substantial research efforts have elucidated a vast and intricate molecular landscape underpinning TRT, laying a foundational blueprint for the rational design and optimization of next-generation targeted radiopharmaceuticals.
At its core, TRT leverages the specificity of molecular targeting agents—such as antibodies, peptides, or small molecules—that conjugate with radionuclides emitting therapeutic radiation. This bespoke method contrasts traditional external beam radiotherapy, providing a systemic approach capable of homing in on disseminated or micro-metastatic tumor deposits with unparalleled accuracy. The molecular precision inherent to TRT represents a quantum leap in cancer therapeutics, as it not only improves the therapeutic window but also opens new frontiers in managing treatment-resistant or inaccessible neoplastic lesions.
A comprehensive appraisal of TRT reveals an enormous diversity of molecular targets currently exploited or under investigation. These targets span from cell surface receptors and tumor-associated antigens to components of the tumor microenvironment (TME), each offering unique vulnerabilities. Recent scientific advances have highlighted how the heterogeneous and immunosuppressive nature of the TME can be co-opted or disrupted by TRT strategies, thereby expanding therapeutic scope beyond mere cancer cell eradication to potentially modulating the tumor milieu itself. This nuanced approach capitalizes on emergent insights into cellular signaling pathways, tumor metabolism, and immune evasion mechanisms.
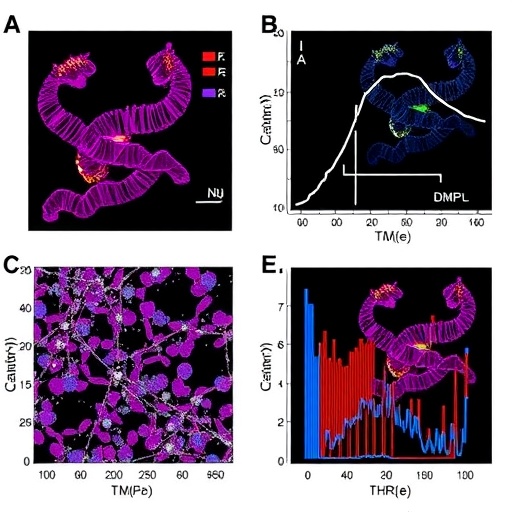
Translating the intricacies of molecular interactions into clinically effective TRT agents requires sophisticated radionuclide conjugation technologies coupled with an in-depth understanding of radiobiology. Radionuclides used in TRT typically emit alpha or beta particles, each characterized by distinct linear energy transfer (LET) profiles and tissue penetration capabilities that influence therapeutic efficacy and side-effect profiles. For instance, alpha-emitters confer highly localized, high-LET radiation lethal to single cells or microclusters, whereas beta-emitters penetrate deeper tissues with broader cytotoxic effects. Optimizing radionuclide selection based on target biology, tumor architecture, and disease distribution remains a focal point of ongoing investigation.
From a clinical perspective, TRT holds promise for an array of malignancies including prostate, neuroendocrine, hematologic, and certain solid tumors, with approved agents demonstrating meaningful survival benefits and manageable toxicity. Notably, the recent success of prostate-specific membrane antigen (PSMA)-targeted therapies has galvanized interest in expanding TRT to other molecularly defined cancer subsets. However, the pathway from bench to bedside is fraught with challenges encompassing production scalability, regulatory hurdles, dosimetry intricacies, and patient selection criteria.
One formidable obstacle in the clinical deployment of TRT is the optimization of dosimetry to maximize tumor radiation dose while sparing normal tissue—a process complicated by the heterogeneous distribution of radiopharmaceuticals and dynamic biological clearance. Advanced imaging techniques, including positron emission tomography (PET) and single-photon emission computed tomography (SPECT), enable real-time tracking of radiotracer biodistribution, informing personalized dosimetry models. Such integrative approaches are pivotal for tailoring treatment regimens and enhancing therapeutic indices.
Furthermore, the molecular design of targeting moieties profoundly influences TRT efficacy. Antibody fragments and peptides offer advantages in tissue penetration and rapid clearance, reducing background radiation and toxicity compared to full-length antibodies. The development of novel linkers and chelators enhances radionuclide stability and delivery precision, underscoring the interdisciplinary nature of this field at the crossroads of chemistry, molecular biology, and nuclear medicine.
Beyond targeting malignant cells, emerging strategies seek to exploit the tumor microenvironment’s unique characteristics—such as aberrant vasculature, hypoxia, and immunosuppressive cell populations—as therapeutic entry points. For example, agents that target fibroblast activation protein (FAP), prevalent in cancer-associated fibroblasts, represent a growing area of TRT research, offering a means to disrupt tumor stroma and augment conventional therapies.
The immunomodulatory potential of TRT also garners considerable attention. Low doses of localized radiation can stimulate antigen presentation and immune cell infiltration, thereby synergizing with immunotherapies such as immune checkpoint inhibitors. This intersection heralds a new era of combinatorial regimens designed to overcome resistance and induce durable antitumor immunity.
Technological advancements have further accelerated TRT innovation. Automating radionuclide synthesis, developing modular radiopharmaceutical platforms, and enhancing preclinical models facilitate rapid identification and validation of candidate agents. Concurrently, big data analytics and artificial intelligence promise to refine patient stratification and predict therapeutic responses, fostering precision oncology.
Nevertheless, widespread adoption of TRT necessitates addressing logistic and economic barriers, including radionuclide availability, specialized infrastructure for handling radioactive materials, and reimbursement frameworks. Collaborative efforts among academia, industry, regulatory bodies, and healthcare systems are critical to surmount these obstacles and translate scientific breakthroughs into accessible patient treatments.
As the molecular blueprint of TRT continues to expand, so too does the potential for this modality to be tailored at the individual patient level. Genomic and proteomic profiling could soon enable the identification of ideal tumor targets and the design of bespoke radionuclide therapies, aligning with the broader vision of personalized medicine. Such adaptability is key to enhancing efficacy across heterogeneous tumor types and dynamic disease states.
In summary, targeted radionuclide therapy embodies a confluence of molecular precision, radiotherapy’s cytotoxic power, and the transformative prospects of personalized oncology. Ongoing research delineates the complex interplay between tumor biology, radiopharmaceutical chemistry, and dosimetry, charting a course toward novel, effective, and safe interventions. As TRT technology matures and clinical frameworks evolve, it stands poised to redefine cancer treatment paradigms, offering hope for improved outcomes across a broad spectrum of malignancies.
The future trajectory of TRT is luminous, driven by interdisciplinary innovation and an unwavering commitment to translating molecular insights into tangible patient benefits. By bridging fundamental research with real-world application, this field exemplifies the frontier of cancer therapeutics, where the molecular underpinnings of disease inform precise, impactful interventions. As the oncology community embraces this therapeutic revolution, patients may increasingly experience the benefits of treatments finely tuned to the molecular and microenvironmental idiosyncrasies of their cancers.
Continued investment in basic and translational research, coupled with clinical trial rigor, will be instrumental in surmounting current challenges and harnessing the full potential of targeted radionuclide therapy. Collaboration across scientific, clinical, and technological domains remains paramount as this elegant approach unfolds from promising concept to standard of care, catalyzing new hope for cancer patients worldwide.
Subject of Research: Targeted Radionuclide Therapy in Oncology
Article Title: The molecular blueprint of targeted radionuclide therapy
Article References:
Primac, I., Tabury, K., Tasdogan, A. et al. The molecular blueprint of targeted radionuclide therapy. Nat Rev Clin Oncol (2025). https://doi.org/10.1038/s41571-025-01069-z
Image Credits: AI Generated
Tags: innovative oncology approachesminimizing systemic toxicity in cancer therapymolecular targeting in cancer treatmentnext-generation cancer treatmentsovercoming treatment-resistant tumorspersonalized cancer therapeuticsprecision oncology advancementsradiopharmaceutical developmentselective radiation delivery mechanismstargeted radionuclide therapytargeting tumor-associated antigenstherapeutic radiation and healthy tissue preservation


 6 hours ago
13
6 hours ago
13

















 English (US) ·
English (US) ·  French (CA) ·
French (CA) ·